One School, Two Sites
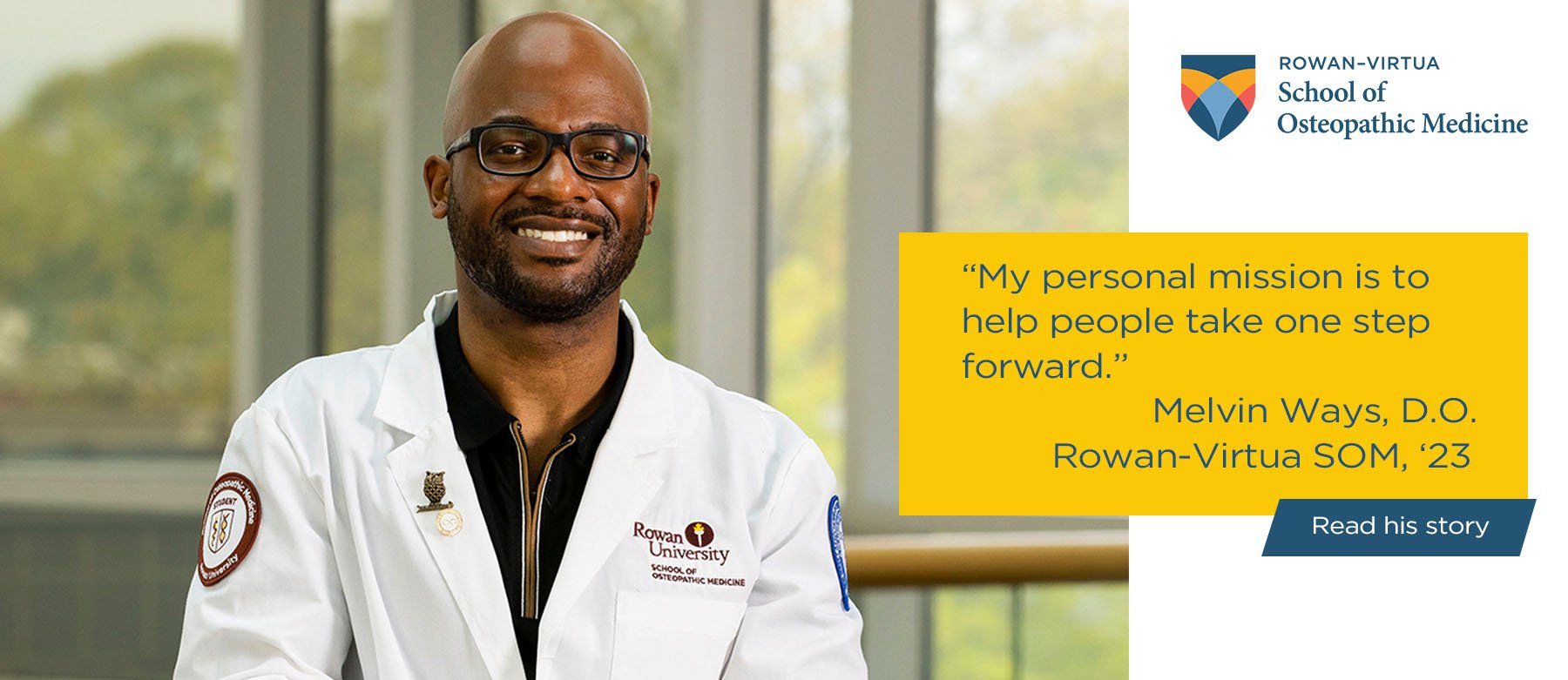
Welcome to Rowan-Virtua SOM
Rowan-Virtua School of Osteopathic Medicine prepares future physicians and scientists who are committed to improving health in New Jersey and throughout the nation. To advance our mission we: develop clinically skillful, compassionate and culturally competent physicians from diverse backgrounds who are grounded in our osteopathic philosophy and ready to meet future healthcare workforce needs; advance research, innovation and discovery to improve health and solve the medical challenges of today and the future; and we provide exceptional patient-centered care, with an emphasis on primary and interprofessional team-based care that responds to the needs of the community including underserved and special needs populations.